Executive summary for Series 6: 3-11 September 2020
This is the sixth of the national surveys of New Zealand general practice experience with COVID-19 and its aftermath. This survey was launched when Auckland was in alert level 2.5, and the rest of New Zealand at alert level 2, due to a cluster outbreak from an unknown source.
Policy recommendations based on responses
Vulnerable patients are increasingly suffering the ongoing effects of COVID-19. These are from delayed or absent non-COVID-19 medical appointments, anxiety and negative life factors such as isolation, financial hardship, food insecurity and domestic violence. COVID-19 policies and restrictions are also disproportionately effecting those who are medical and economically vulnerable, and these populations need additional support.
Effects of COVID-19 on practices
The strain on practices from COVID-19 continues, with 86% reporting significant to severe impact (90% in S5), and 2% reporting no ongoing effect. 20% still report ongoing effects of COVID-19 leading to staff layoff or affecting leave arrangements (similar to 20% in S4 and 18% in S5).
Effects on vulnerable patients
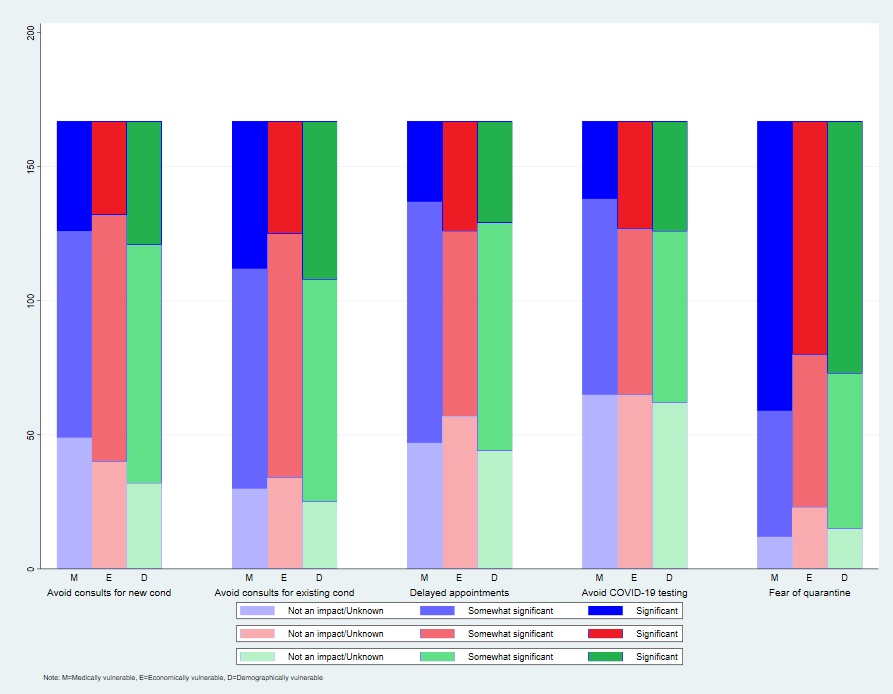
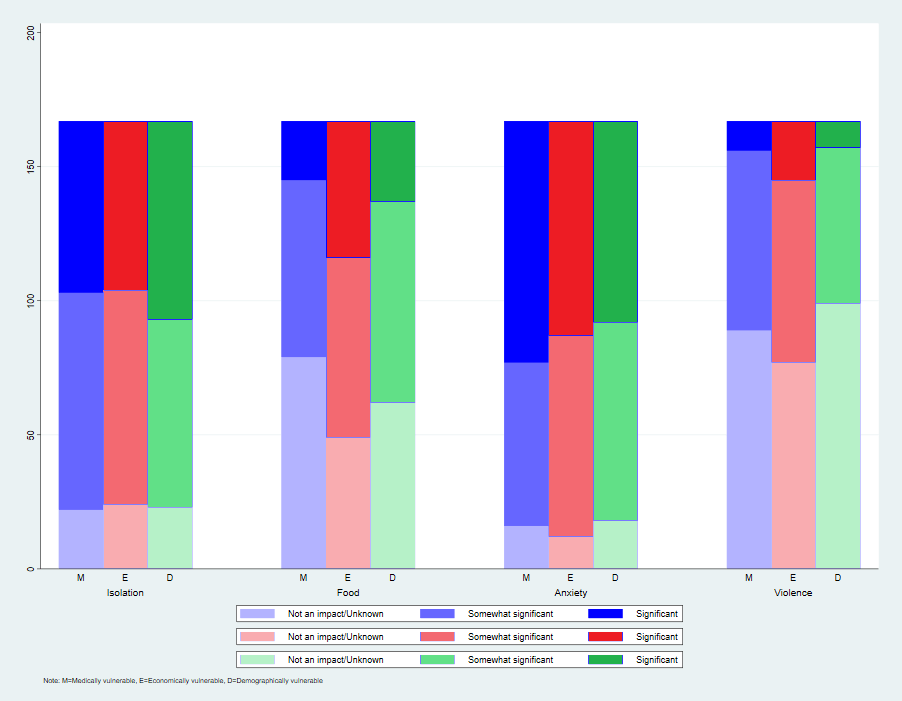
This survey focused on COVID-19 effects on patients who are medically (eg type-2 diabetes, immune compromised), economically (eg living in poverty, unemployed, underemployed, recently lost job, casual worker) and demographically (Māori, Pacific, migrant, elderly, in aged care) vulnerable. Respondents thought that delayed hospital admissions (93%) and avoiding consultations for new (71%) and existing (82%) conditions are impacting significantly on their medically vulnerable patients. For the economically vulnerable, risk of domestic violence (54%) is a big issue, as is fear of quarantine (63%) for the demographically vulnerable. Anxiety (90%, 72%, 89%), isolation and loneliness (87%, 86%, 86%) are impacting on all groups.
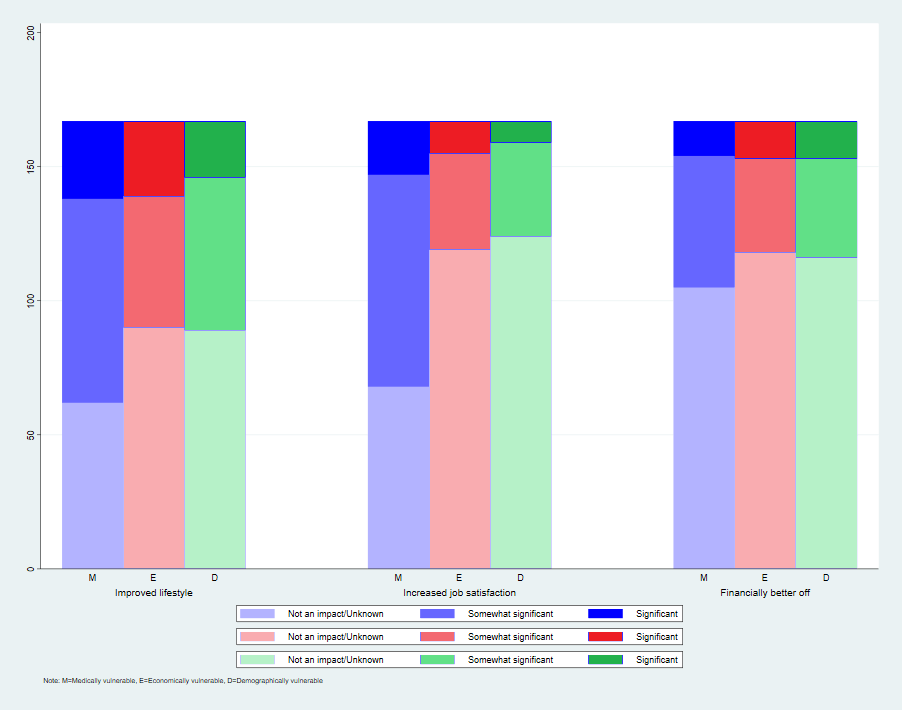
Improved lifestyle choices in some patients (increased physical activity, home cooked meals, family time) resulting from COVID-19 are seen mostly in the medically vulnerable (63%), as is Increased job satisfaction by working from home (59%), and being financially better off through less spending, government support, increased income (37%).
Conspiracy theories
For the first time, respondents mention concerns about some patients presenting with conspiracy theories:
“Have encountered some patients with fixed ideas about conspiracy theories” [GP]
“Concerning comments in a couple of people about conspiracy theories resulting in failure to take responsibility to protect themselves or others ( mask wearing and lockdown measures)” [GP]
Testing
37% of practices are now experiencing challenges in getting PPE, and there are concerns that primary care is missing out: “We need appropriate PPE supply rather than only if the DHB can spare it – we are seeing the bulk of patients with respiratory symptoms so need the bulk of PPE” and “PE request denied by DHB”. This cost is falling on some practices: “PPE no longer supplied to us and we have to buy our own to do testing” but this appears to be DHB-dependent, as another writes “Excellent PPE and swab supply.”
Telehealth consultations
65% now report they have patients who struggle with telehealth under the current raised alert levels (increased from 55% in S5). Video consultations are being conducted in 42% telephone consults in almost all (95%) – for 55 % this is for more than 20% of consultations (as per S5), and other types of e-consultations (eg email or patient portal) in 46%. A number of respondents highlight the value they find in telehealth. One GP writes: “enjoyed the telconsults and have found the tech changes that have enabled this to be good; I realise that face to face care is not always necessary in an established medical-patient relationship; telemedicine saves the patient time (no more travelling, waiting for the Dr, the consult, then the drive to the pharmacy , waiting for script to be made up, drive home- 1 hour or more); the teleconsult process can be very efficient in consultation dx and ordering X-rays / labs/ scripts/ referrals all done while speaking to the pt on a head set”.
Morale
The positive effects of dealing with COVID-19 on the practice team and other providers continues to be highlighted:
“Positive is pulling together and alliance of differing community providers” [GP]
“Overall it has been a very positive experience with both patients and staff all bonding over the shared challenges and creating new ways of managing medical needs” [GP] Some practices praise their patients on their understanding:
“Patients in general have been understanding & compliant” [PM]
“We have great population here all very kind and understanding” [GP] However others comment on the ongoing strain:
“We are starting to show signs of burnout- in all team members. Patients are irritable too” [PN]
“The whole team is really tired” [GP]
Financial considerations
20% still report lack of recompense for testing: “It would be nice to receive the payments for swabs taken over the past 4 months. Last payment received was 13/05/2020. Nil since”. 8% currently have financial barriers to acquiring PPE but some are now worried: “New fear is the news that MOH/DHBs are going to stop supplying PPE to primary care which will add to our financial and emotional burden”. 45% now reporting large drop in patient volume: “patient numbers attending markedly down, affecting viability of the clinic and it’s ability to employ our long term doctors”
Method
On Thursday 3 rdSeptember, the sixth of the fortnightly Quick COVID-19 NZ Primary Care Survey was launched. An invitation to participate was distributed to general practice GPs, nurses and managers across the country, disseminated by the RNZCGP, RNZCUC, GPNZ, PMAANZ, RGPN, and NZMA. The survey closed on 11 September.
Sample
There were 167 respondents: 120 doctors (GPs or urgent care doctors), 19 practice nurses [PN], 5 nurse practitioners (NP], and 23 practice managers [PM]. 67% of practices were GP-owned; 74% had more than 3 GPs; 32% independent and part of a larger group, 2% were DHB owned, 16% owned by a community trust, and 25% as urgent care / after hours. 25% identified as rural.